Text chosen by Janice M. Bell – Design by Bryce Mee
What’s in a name?
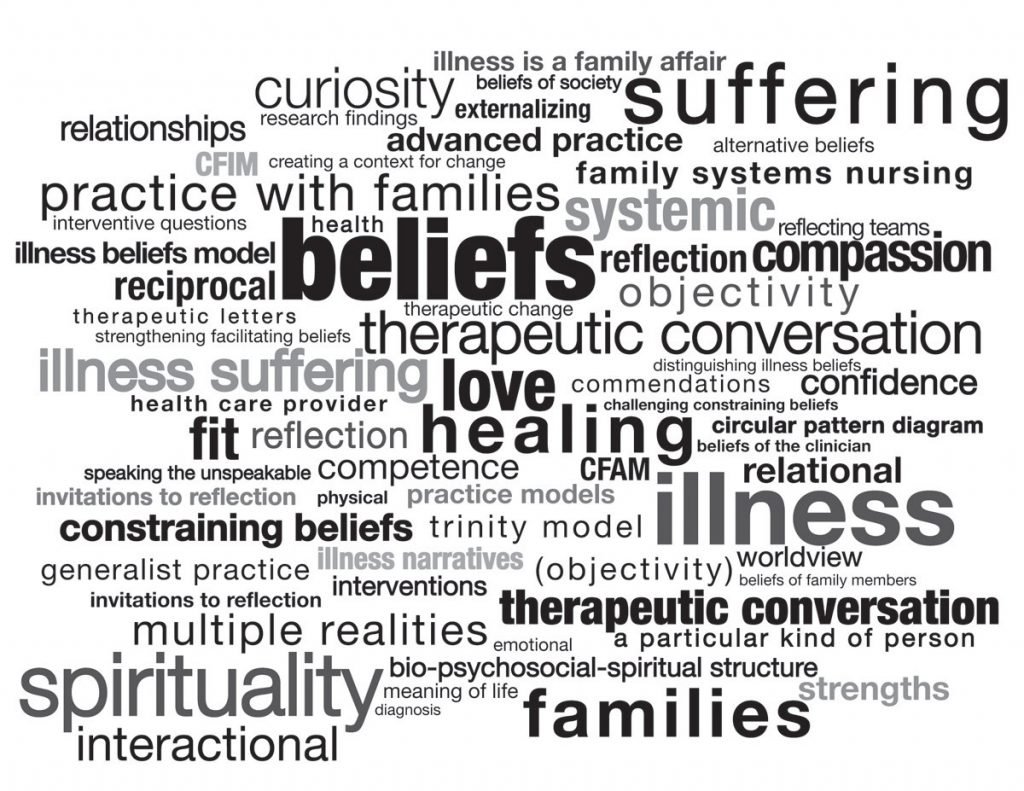
I’ve been doing a lot thinking lately about what to call practice with families that addresses experiences of health and illness. Some call it family focused practice, family friendly practice, family centered practice, family health and healing, relational practice, family nursing, Family Systems Nursing, systemic health care, family medicine, medical family therapy, medical social work, etc. In order for the practice name to fit for me, it needs to honor the following distinctions:
1. The focus of the practice is on sustaining health and promoting healing while directing practice towards both health promotion and illness suffering. For example, addressing a mother’s illness suffering within a family meeting can be health promoting for generations to come.
2. The practice recognizes that relationships between people (especially significant relationships with people who give a damn about you) reciprocally influence health/illness.This means that the way you and I get along together (or don’t) affects my cells and my soul and if illness arises in me, you and our relationship together will likely be affected too–“for better or worse”.
3. I’ve believed for a long time that the word “family” in family practice is a misnomer. The key participants include a variety of systems levels: individuals, family members, whole family units, AND health care providers, health care systems, and the larger societal and cultural systems within which these individuals and groups of individuals are nested.
4. The practitioner (a.k.a. clinician) is adept at assessing multiple systems levels (see #3) and choosing interventions which target the systems level(s) that offers the greatest possibility for health and healing, i.e., should the intervention target the individual, the relationship between two or more family members, the relationship between the family and the health care providers, societal beliefs and behavior, or some combination of these? One clinical practice model that offers a conceptual map for addressing the intersection of beliefs at these multiple systems levels is the Illness Beliefs Model (Wright & Bell, 2009)
5. The practice occurs in a relationship between an individual(s) and a nonjudgmental clinician who prefers collaborative, non-hierarchical relationships and who believes in the legitimacy of multiple realities. A strengths based orientation of the clinician moves the therapeutic conversation towards family competencies and strengths rather than towards deficits and pathology. The proponents of family centered care argue that respect, information, and partnership with families in decision-making are hallmarks of “good” practice with families–however what is missing for me in this practice description is a willingness and competence to address illness suffering and family healing as well.
My history is situated within the disciplines of nursing and psychology and immersed in the specialization of family nursing. My “clients” are frequently learners–who are or will be practitioners of health care.I prefer the term “Family Systems Nursing” at the moment.I believe Family Systems Nursing best addresses the distinctions listed above. What about you? What do you prefer to call this kind of practice with families?
For more information on this topic, please see an Editorial I wrote for the Journal of Family Nursing: “Family Systems Nursing: Re-examined”. I’d also recommend another Editorial that I wrote for the Journal of Family Nursing called “Family Nursing is More than Family Centered Care“.
References:
Bell, J.M. (2009). Family Systems Nursing re-examined [Editorial]. Journal of Family Nursing, 15(2), 123-129. doi:10.1177/1074840709335533
Bell, J. M. (2013). Family nursing is more than family centered care [Editorial]. Journal of Family Nursing, 19(4), 411-417. doi:10.1177/1074840713512750
Wright, L.M., & Bell, J.M. (2009). Beliefs and illness: A model for healing. Calgary, Alberta, Canada: 4th Floor Press. Kindle version available from Amazon.com